Cornual (interstitial) ectopic pregnancy
Cornual ectopic pregnancy may be managed medically just like tubal ectopic pregnancy
In properly selected cases of cornual ectopic pregnancy, injecting methotrexate into the gestation sac is a treatment choice
The same is true for Cesarean scar and cervical ectopic pregnancies
Ms. Valdez was pregnant after frozen embryo transfer of an euploid embryo. The viability of the pregnancy was confirmed on the 6 2/7 weeks ultrasound. The second ultrasound showed the viable 7+ weeks pregnancy was a right cornual ectopic pregnancy. She was given two options: surgery by minimal invasive surgeons or medical treatment (injecting methotrexate to the gestation sac). She opted for the latter.
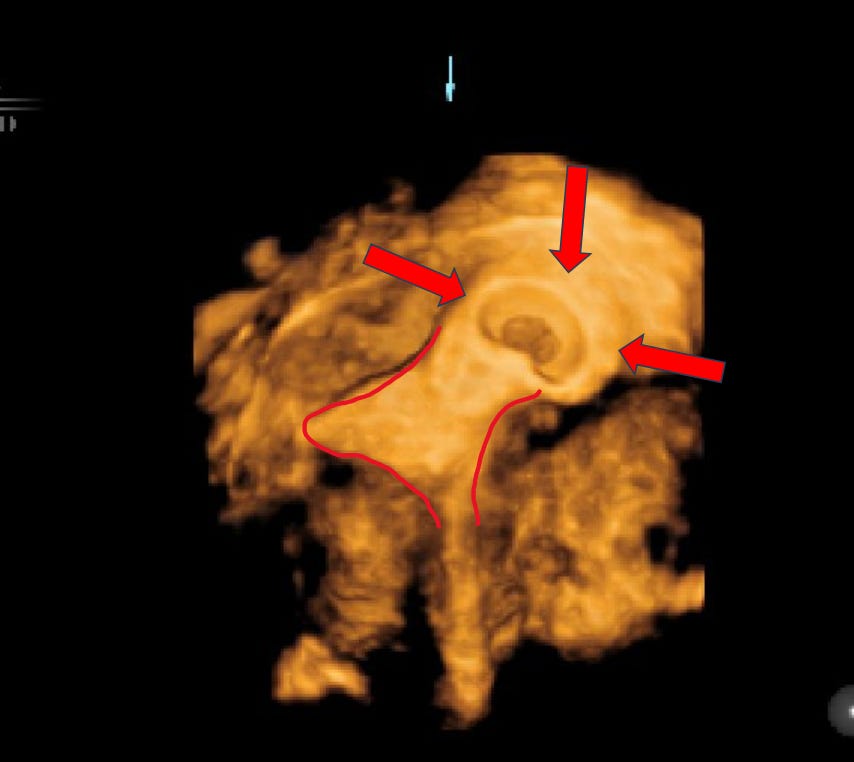
Under IV general anesthesia and real-time trans-vaginal ultrasound guidance, KCl was injected to stop the fetal heart. After that, 100 mg methotrexate was injected into the gestation sac. The procedure took 20 minutes with barely any blood loss. She was given precautions and discharged home a few hours later.
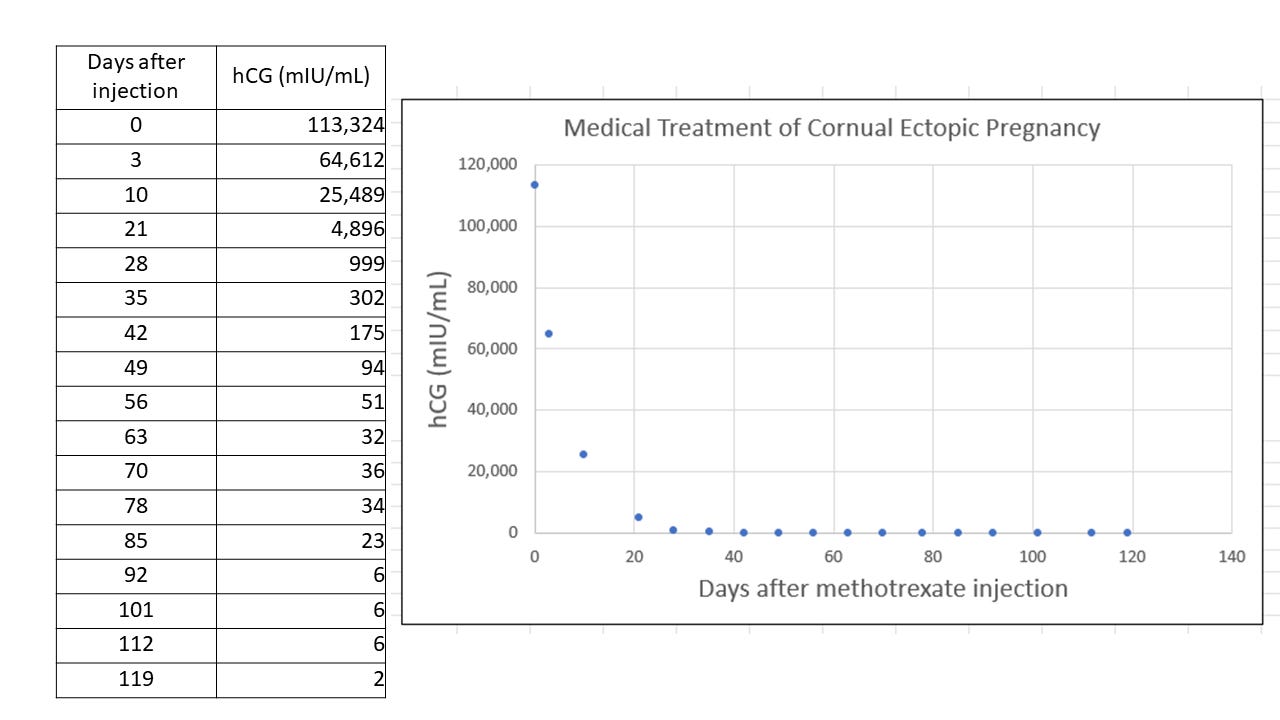
On the day of methotrexate injection, her hCG was 113,324 mIU/mL. One hundred and nineteen (119) days later, her hCG was 2 mIU/mL. She had no complaints during the 119-day follow-up.
Cornual ectopic pregnancy is different from tubal ectopic pregnancy
Compared with tubal ectopic pregnancy, cornual ectopic pregnancy has following features:
It is rare: cornual ectopic pregnancy consists of 2 – 4 % of all ectopic pregnancies.
It usually ruptures during the second trimester (vs 7 - 9 weeks for tubal ectopic pregnancy).
It may be diagnosed as early as 7 weeks gestation, allowing ample time to plan management.
Once it ruptures, shock follows within minutes due to massive internal bleeding.
Surgery is associated with (usually massive) bleeding and removal of part of the uterus.
A laparotomy is usually needed - few surgeons have the skill to perform laparoscopy.
My personal experience
Given the above, medical treatment becomes an attractive choice. I have, over the last decade, injected methotrexate directly to the gestation sacs of 15 - 20 rare ectopic pregnancies, including cornual ectopic, Cesarean scar ectopic and one cervical ectopic pregnancy.
Thus far, no one needed surgery or a second dose of methotrexate. Also, no one reported pelvic pain or heavy vaginal bleeding – except the one with cervical ectopic pregnancy. This patient had heavy vaginal bleeding as the pregnancy was being aborted.
A handful of patients had a hystero-salpingography (HSG) several months after negative hCG. The tube used to harbor the cornual ectopic pregnancy was confirmed patent – similar to tubes harboring tubal ectopic pregnancy treated with IM (intramuscular) methotrexate.
My limited experience is a proof of concept that these rare ectopic pregnancies may be managed medically by injecting methotrexate directly into the gestation sac. I was prepared to perform surgery on any one who needed it. Fortunately, there was none.
hCG levels after direct methotrexate injection
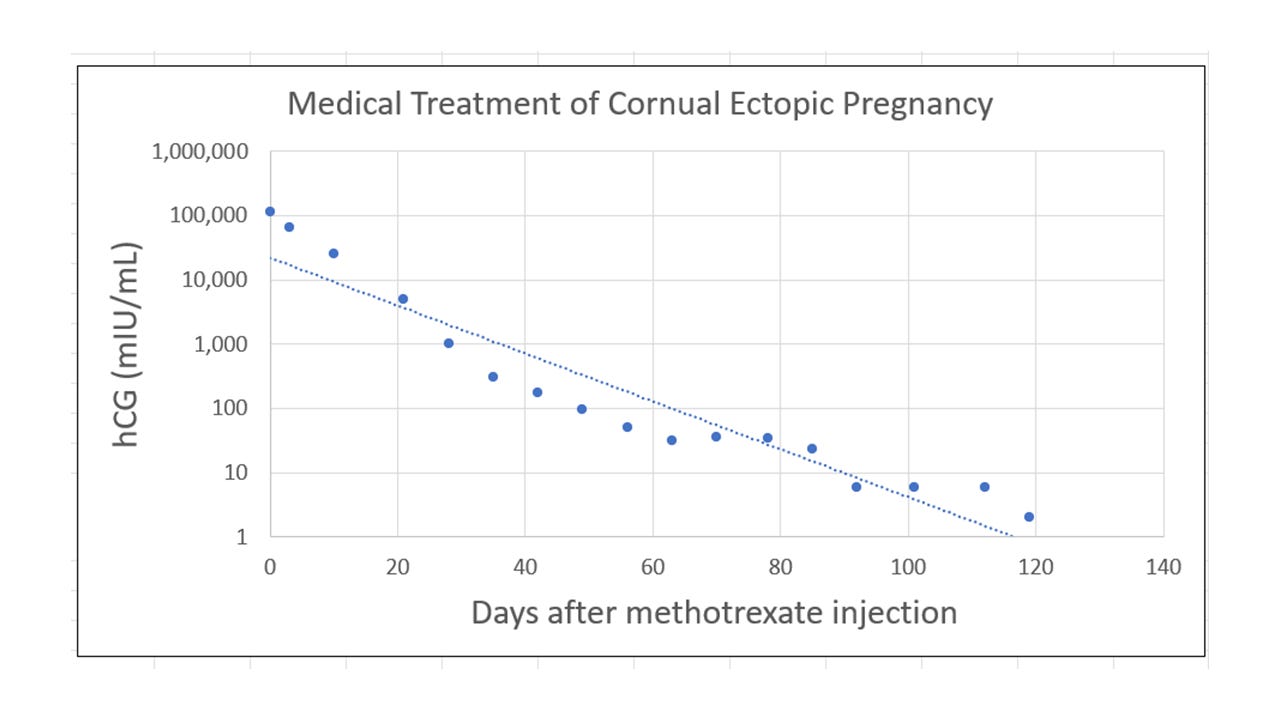
After injecting methotrexate to the gestation sac, precipitous hCG drop is expected in as early as three days. In Ms. Valdez’s case, the reduction was near 50% (from 113,324 to 64,612 mIU/mL). Similar degree of decrease is not usually seen in individuals with tubal ectopic pregnancy receiving IM methotrexate injection. In most instances, hCG continues to rise for 3 - 4 days after IM injection.
After the precipitous drop, hCG levels decrease exponentially. It decreases at a rate proportionate to its most recent (current) value, essentially following the elimination half-life of hCG. The value of hCG on any given day after injection can be expressed as Y = 22078e-0.086X (Y = initial hCG value, X = days after injection, R2 = 0.9515).
Thus, the hCG value on the day of treatment has great impact on how long it takes to reach negative hCG. It is not unusual to take up to 3–4 months. In Ms. Valdez’s case, it took 119 days. Her hCG on the day of injection was 113,324 mIU/mL.
Finally
The REI (reproductive endocrinology and infertility) and MIS (minimal invasive surgery) services of Baylor College of Medicine, Department of Obstetrics and Gynecology combine their effort to offer comprehensive service to individuals who have rare ectopic pregnancies, including cornual, Cesarean scar, and cervical ectopic pregnancy.
The REI service evaluates the suitability of medical treatment and provides the treatment; the MIS service is the surgical backup. Both services are at the Texas Children’s Pavilion for Women in the Texas Medical Center, Houston, TX.
We welcome patients from the greater Houston area as well as outside the Houston metropolis – as long as patient’s condition is considered safe to travel by their provider. As mentioned earlier, there is ample time to plan treatment if a diagnosis of cornual ectopic pregnancy is confirmed in the first trimester. Initial consultation may be made via a video conference.


