Common IVF stimulation protocols
Two common stimulation protocols use different agents to contain the pituitary gland
After reading the overview of IVF treatment, medical student Susan asked what are common protocols used in IVF and how are they used.
IVF is a process of attrition. More eggs mean higher chance of success. Therefore, the first goal in IVF is to retrieve as many eggs as possible (and safely). This is the so-called COS, “controlled ovarian stimulation”. It is carried out by FSH injection, such as GonalF®, Follistim®, or Menopur® (which has 1:1 ratio of FSH and LH).
In order to have the highest number of mature follicles (and mature eggs), a second medication is used to prevent premature LH surge by the pituitary gland. Uncontrolled, premature LH surge ruptures both mature and immature follicles, reducing the number of mature eggs. To suppress premature LH surge, GnRH (gonadotropin releasing hormone) agonists (such as Lupron®) or antagonists (such as Cetrotide®) are added to the regimen. Immature eggs cannot be fertilized by sperm, and the today’s technology cannot make them mature once removed from the ovary.
GnRH agonist stimulates, and GnRH antagonist inhibits the pituitary gland. The antagonist’s stimulatory effects become inhibitory after it is administered daily for 5-7 days. In contrast, the inhibitory effect of the antagonist is immediate, and the full effect is seen within 24 hours.
All IVF stimulation protocols need FSH (and LH). They differ in how to suppress the premature LH surge. Protocols using GnRH agonist and GnRH antagonist are two common IVF stimulation protocols. The former is also called the “long” protocol, and the latter, the “short” protocol. Other, less common protocols use micro-Lupron®, clomiphene citrate or letrozole.
GnRH agonist protocol (the “long” protocol)
This is the protocol used in the early days of IVF, because GnRH antagonist was not available then. A typical GnRH agonist protocol begins with Lupron® injection on cycle day 21 of the earlier cycle. About 7-10 days later, when the menstruation begins, a base line ultrasound and blood tests are performed. Once follicles/cysts of the ovary are < 10 mm and the estradiol is < 50 pg/ml, FSH injection begins. Lupron® continues till the day of trigger shot.
GnRH antagonist protocol (the “short” protocol)
In the GnRH antagonist protocol, FSH is started on the third evening of menstruation after a baseline ultrasound confirming all follicles/cysts are < 10 mm. Typically, the antagonist is added to the regimen on the 6th evening of stimulation or when the lead follicle is 12 mm. The antagonist is administered once daily until the day of trigger.
Compared with the agonist protocol, the antagonist protocol is nicknamed the “short” protocol, because it does not need the 5-7 days to suppress the pituitary gland.
Monitoring
Ultrasound exams and blood tests are used to watch the progress of COS. The ultrasound shows the physical response of the ovary, the size of the follicle. The blood test (estradiol) shows the chemical response of the ovary. IVF docs adjust medication or decide on the addition of the antagonist based on the results.
The first monitoring visit typically takes place after three days of FSH injection. The remaining visits typically take place every other day. Occasionally, the follow-up intervals are increased or decreased based on the response.
Birth control pills and IVF stimulation protocols
For logistical reasons (to accommodate patient’s work or travel, or the load of the clinic), birth control pills are added to the stimulation protocols. Typically, patients are asked to begin the pill two nights after the menstruation. The duration of the pill varies, from a few days to a couple of weeks (or longer). This delays the start of FSH injection and egg retrieval.
Birth control pills add flexibility to the timing of IVF treatment. But it comes at a price. My personal observation shows more than two weeks of pills is associated with longer days of stimulation before reaching trigger. For example, a typical antagonist stimulation without birth control pills (or less than seven days of pills) takes nine or ten days. If 14 or more days of birth control pills are used, it may take more than 11 days to reach trigger.
Which stimulation protocol?
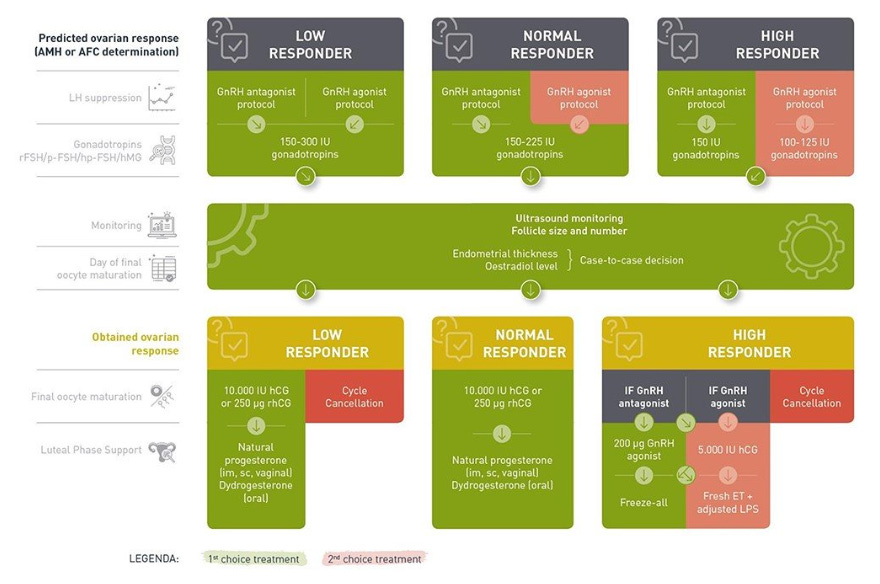
The European Society of Human Reproduction and Embryology (ESHRE) published a guideline on choosing IVF stimulation protocol based on whether the patient is a low responder, normal responder, or high responder based on AMH and antral follicle count and others (Hum Reprod Open. 2020 May 1;2020(2):hoaa009. doi: 10.1093/hropen/hoaa009. eCollection 2020. PMID: 32395637). Its figure is below.
The guideline is a good starting point, but there is room for fine tuning based on individual’s needs/characteristics. For example, all other things being equal, heavier patients need more medication than thinner patients to achieve the same tissue level.
Other stimulation protocols
Micro-Lupron flare, clomiphene citrate (or letrozole) combined with FSH have been used successfully to stimulate the “low responders”. These agents induce the pituitary to secrete endogenous FSH and LH. Exogenous FSH is then added.
Micro-Lupron flare protocol uses 40 micro-gram Lupron twice daily to stimulate the pituitary initially, and down-regulate the pituitary later. Micro-Lupron is started on the first evening of menstruation. FSH injection is started on the third evening of menstruation after baseline ultrasound. For comparison, five to ten times more Lupron (0.5 or 1 mg daily) is used in the “short” protocol.
Clomiphene citrate or letrozole are started on the second or the third day of menstruation in the clomiphene or letrozole and FSH protocol. Daily FSH injection starts three days later - there is two days overlap.
Contrary to the GnRH agonist or antagonist protocols, birth control pills are not allowed in these two protocols because pills turn off the pituitary gland. Therefore, it lacks flexibility in medication start day. IVF docs are “at the mercy” of the ovary - they need to execute the stimulation protocol whenever the menstruation starts.
Adjuvants to stimulation protocol
Not much concrete data exists on adjuvants used in IVF stimulation. These include DHEA, CoQ-10, human growth hormone, and others. I occasionally recommend DHEA and CoQ-10; I do not normally recommend human growth hormone.
Random start stimulation protocol
This protocol is usually reserved for fertility preservation in cancer patients, prior to chemotherapy or irradiation that may wipe out follicles in the ovary. Eggs are retrieved, and eggs (or embryos) are preserved.
The IVF docs are usually given two to three weeks to complete the task. The atagonist protocol is typically used, and as quickly as feasible - irregardless of the state of menstrual cycle. Compared with the typical antagonist protocol, the results are reasonably good.