A 29-year-old patient has bilateral endometrioma and secondary infertility with the same partner
Clear cell carcinoma of the ovary originates from endometrioma
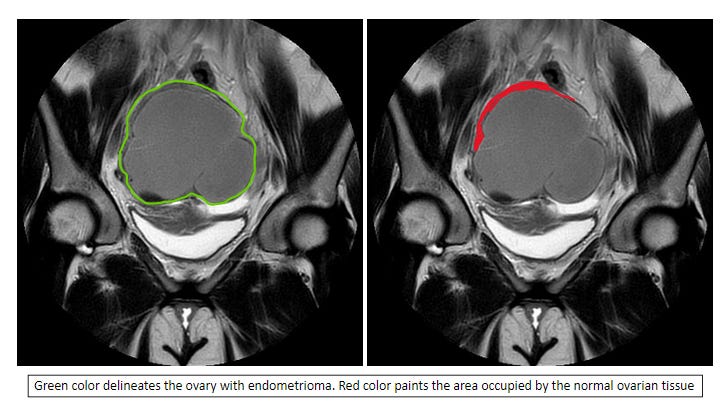
Large endometrioma compresses normal ovarian tissue and compromises ovarian function
Ms. Green is here to discuss management options for the above conditions. She conceived naturally after five months of trial and delivered a boy two years ago. She did not breastfeed or use birth control after the delivery but did not conceive yet. In the last six months she noticed the menstrual cramps worsened. Ultrasound revealed bilateral endometriomas, 4-cm and 5-cm each. Today’s ultrasound shows her total antral follicle count is 17. A minimal invasive surgeon plans to perform cystectomy on both ovaries; oocyte freezing prior to the procedure was brought up during pre-operative counseling.
Knowing the surgeon who is performing the surgery, I assure Ms. Green to proceed with the surgery without oocyte freezing. My recommendation is based on the following consideration:
Ms. Green is experiencing pain.
Endometrioma may rupture spontaneously or during egg retrieval. Content of endometrioma spilled into the pelvis is a medical emergency.
“Endometrioma” is a clinical diagnosis based on images. Endometrioma may give rise to clear cell epithelial cancer of the ovary. This type of ovarian cancer makes up 10% of all epithelial ovarian cancer.
My experience with the surgeon makes me believe Ms. Green will have improved ovarian function after the surgery. Although cystectomy may compromise ovarian function, the mass effect from a 5-cm endometrioma may be more.
Given Ms. Green’s past performance (i.e., conceiving after five months of trial) and today’s total antral follicle count, she may be able to conceive naturally after the surgery – the surgery removes the mass effect on the ovaries (see figure below), and restores the pelvic anatomy.
If IVF (in-vitro fertilization) is needed, I expect her post-surgical ovarian function to be better than today for reasons stated above.
I offered Ms. Green the following plan:
AMH (anti-Mullerian hormone) levels today, and two to three months after the procedure.
HSG (hysterosalpingogram) after the procedure and before she prepares to conceive. This test confirms tubal patency and bestows therapeutic benefits.
Begin IUI (intrauterine insemination) if she does not conceive after six months of trial.
Begin IVF if she does not conceive after three cycles of IUI treatment. IUI treatment may be skipped if so desired.
I gave Ms. Green the above recommendations based on risk and benefit analysis considering her past fertility performance, her symptoms, the size of the endometriomas, and my experience with the surgeon.
Not all patients who have endometrioma need surgery right away. In asymptomatic patients (and with smaller endometrioma, i.e., < 3 cm) who are reluctant to have surgery, I believe IUI and/or IVF are reasonable options. Past reports show hormone therapy (such as Lupron) may reduce the size of smaller endometrioma.